标签:

Hepatitis B virus (HBV) is a double-shelled DNA virus that
can be spread by extremely small volumes of blood and,
as such, is a potential risk during the provision of dental
treatment. Markers of infection include intact virion
(Dane particle), surface antigen (HBsAg) and a breakdown
product of core antigen termed e antigen (HBeAg).
An effective vaccine against HBV is available and dental
students on entry to dental school must show evidence of
protection by adequate antibody titres. Similarly, dental
healthcare workers should maintain an adequate level
of protection. Dental healthcare workers who are found
to have HBeAg should not provide dental treatment.
Hepatitis C virus (HCV) is an enveloped RNA virus that is
mainly spread in blood. The risk of transmission of HCV
during dental treatment is unknown but unlikely. The
presence of HCV is detected on the basis of serological
markers of the virus. An effective vaccine is not available
at the present time. Dental students have to show
evidence of being HCV negative at entry to dental school.
Dental healthcare workers who are found to become
infected with HCV must not provide treatment.
Changes in general health and the treatment
of disease can alter the composition of the oral
microflora. A good example of this is the treatment
of head and neck cancer which can cause
Gram negative enteropathogens to colonize the
mouth and cause destructive changes in bone following
extractions. Drugs such as bisphosphonates
can also cause similar effects on the jaw bones.
Bacteria which are part of the normal commensal
oral microflora can cause infection and destruction
of facial tissue in conditions such as cancrum
oris, particularly if they are not treated and there
is associated malnourishment. Hepatic infections
such a hepatitis B can result in the release of large
quantities of viruses into the saliva which could be
potentially transmitted to health care workers. In
contrast, hepatitis C probably does not get into the
oral cavity to cause an infectious risk. Similarly,
on present evidence, prions, the agents thought
to be responsible for CJD and other transmissible
spongiform encephalopathies, probably are
not transmissible through saliva, but may be present
in other oral tissues necessitating some dental
instruments being single use items and disposed
of after use. Sexually transmissible diseases such
as syphilis and gonorrhoea can cause oral lesions,
as can tuberculosis, and are potentially transmissible
through saliva. Thus, effective infection control
strategies are needed (Ch. 12).
There are problems in categorizing which level of
infection control is appropriate for dentistry. Many of
the patients who attend dental surgeries may asymptomatically
carry potentially infectious diseases but
they do not know they are infected (e.g. hepatitis
B or C). The risk of transmission could be high in
dentistry if there is blood to blood contact through,
for example, an inoculation (sharps) injury. In addition,
the major fluids encountered in dentistry
areblood and saliva and these could potentially transmit
infectious disease. The risk for most of the surgical
procedures done in dentistry, therefore, is in the
medium category. Since most dental patients who
asymptomatically carry disease are unaware of their
infectious status it is wise to treat everyone with
the same precautions; these are often described as
Standard or Universal Precautions.
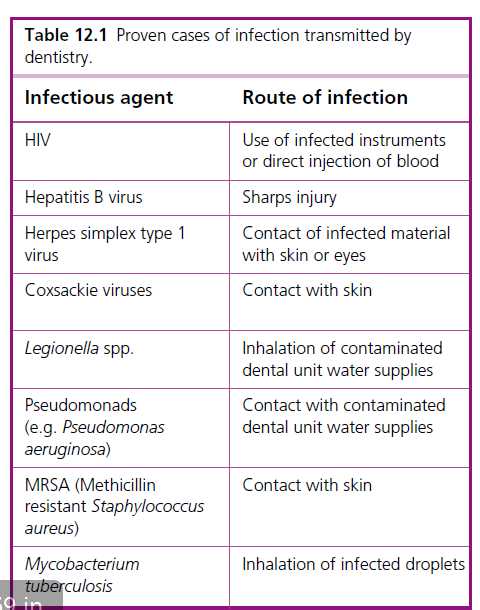
The number of proven cases of infectious diseases
that have been transmitted by dental personnel,
treatment or patients is very limited and the diseases
are listed in Table 12.1. The pathogens include
Mycobacterium tuberculosis (the causative organism
of the majority of cases of tuberculosis in humans),
methicillin resistant Staphylococcus aureus (MRSA),
Pseudomonas spp., and the hand, foot and mouth
virus (Ch. 10), and their transmission has resulted
in serious, but not life-threatening infections. The
list also includes infections caused by Legionella spp.
and hepatitis B virus which have resulted in death of
Immunization
The protection of dental personnel by immunization
before they engage in dental procedures is
an important part of infection control. Nowadays,
many regulatory authorities require that dentists,
nurses, hygienists and therapists are not carrying any
potentially infectious disease before they undertake
or assist with any dental procedures. Freedom from
infectious disease and satisfactory records of immunization
should be a contractual prerequisite before
dental personnel are employed. The vaccinations
required are listed in Table 12.2 and many of these
are done routinely in adolescence. The exception to
this is hepatitis B vaccination which needs to be satisfactorily
completed before any exposure to surgical
procedures is done.
Inoculation injuries (often called sharps or needlestick
injuries) have a high potential for the transmission
of serious infection as they can involve blood
to blood contact. They must be avoided by careful
needle resheathing techniques and safe disposal of
sharps. The two occasions when they are most likely
to occur are during the resheathing of local anaesthetic
equipment and the removal and decontamination
of used dental instruments. A schema for
dealing with sharps injuries is shown in Fig. 12.5.
After immediate first aid the injured person should
be assessed and hepatitis B and/or HIV prophylaxis
should be considered. An audit of the reasons for
the sharps injury should always be done and surgery
protocols modified to prevent it happening again.
Hepatitis B
This virus can be found in the blood of patients who
are infected. It consists of a double-layered coat which
contains an important glycoprotein called hepatitis
B surface antigen (HBsAg), which is often used
to detect whether or not a patient has been exposed
to the virus. Inside the coat is another glycoprotein
called the hepatitis core antigen (HBcAg). There
is another antigen from the virus called hepatitis B
e antigen (HBeAg) which is used to assess whether
a patient has active disease. The period taken from
inoculation of this virus to the development of symptoms
is long and can be up to 8 weeks. The majority
of patients (over 60%) who contract hepatitis carry it
asymptomatically and eventually overcome the disease.
Even though they may be asymptomatic, HBsAg
and HBeAg can be detected in their blood. Patients
who develop symptoms may become chronic carriers,
develop cirrhosis or have acute illness and, in a
minority of cases, die. There are no precise figures as
to how many people carry hepatitis B worldwide but
in some countries as many as 5% are known to have
been exposed to this virus. Patients who have hepatitis
will release intact hepatitis B into saliva where it
could potentially be a source of cross infection. It has
been estimated that 0.0001 ml of blood could transmit
the disease. The primary route of transmission of
hepatitis B is sexual, but blood to blood transmission
in unvaccinated persons has a 40% transmission rate.
An effective vaccine against this disease is available.
标签:
原文地址:http://www.cnblogs.com/biopy/p/4298364.html